Cardiovascular diseases are a group of disorders of the heart and blood vessels and are the leading cause of death globally. Heart attacks and strokes account for 80% of these deaths and are primarily related to atherosclerosis, a condition resulting from the buildup of plaques in the arteries. Vascular grafts made of expanded Teflon (ePTFE) or Dacron fabric are widely used for cardiovascular reconstruction to overcome these blocks.
Clinically, a 3- to 4-mm graft is required for peripheral limb repair and a 2- to 3-mm-diameter graft would be invaluable for coronary artery repair. However, there are no FDA-approved grafts ≤4 mm in diameter since they all fail primarily due to thrombosis.1 A promising alternative is to fabricate viable vascular grafts using electrospun fibers. These small tubular structures can be designed with anti-thrombogenic materials for properly restoring blood flow.
Vascular disease:
Vascular diseases, specifically coronary and periphery artery diseases are the highest cause of mortality worldwide, estimated to increase to 23.3 million by 2030 .2 Vascular diseases are primarily caused by the narrowing of the blood vessels from atherosclerosis, and plaque buildup within the artery walls.3 Replacement of the blood vessel is a common corrective measure to properly restore blood flow within the diseased tissue.
For large blood vessels, a common way to treat vascular diseases is by incorporating synthetic bypass grafts typically made from expanded polytetrafluoroethylene (ePTFE). However, if the ePTFE graft inner diameter is lower than 6 mm, the graft will cause thrombosis and fail. In such cases, autologous grafts are the preferred recourse. In addition to being in limited supply, the use of vascular allografts and xenografts is prone to inducing an immune response and requires the patient to take immunosuppressants.4 With these complications in mind, it is imperative to design alternative grafts that are anti-thrombogenic and be tuned in size for small-diameter vessels. Electrospinning is a versatile strategy that can be utilized for generating small-diameter tubular structures that mimic the structure of the extracellular matrix and can include incorporated materials that have innate anti-thrombogenic properties.5
Electrospinning for Promoting Vascularization:
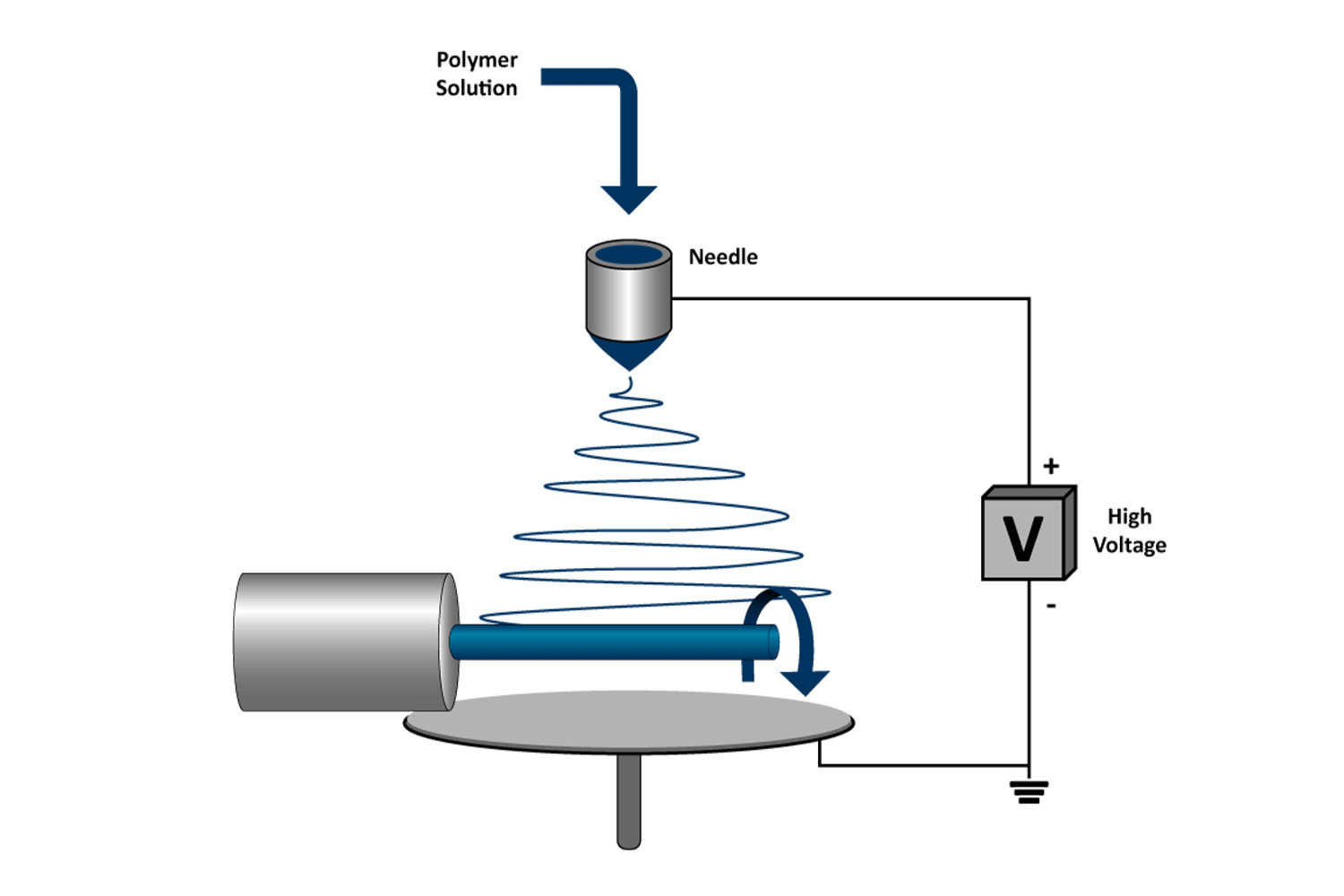
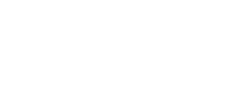
Electrospinning is a process by which a polymer solution is extruded into a high-voltage field and propelled toward a grounded or negatively charged collector. During the time of flight, the solvents evaporate, and the polymer is collected in the form of nanofibers (Figure 1A). The solution formulation can be tuned for generating electrospun fibers that range from 100 nm to a few microns. Furthermore, the electrospinning parameters can be tuned to control fiber alignment in random, semi-aligned, or aligned orientations.6 Due to its ability to fabricate nanofibrous structures, electrospinning is a promising technique to develop scaffolds that mimic the native structure of the extracellular matrix. Further, previous work has fabricated electrospun fibers naturally resistant to thrombosis. 7,8
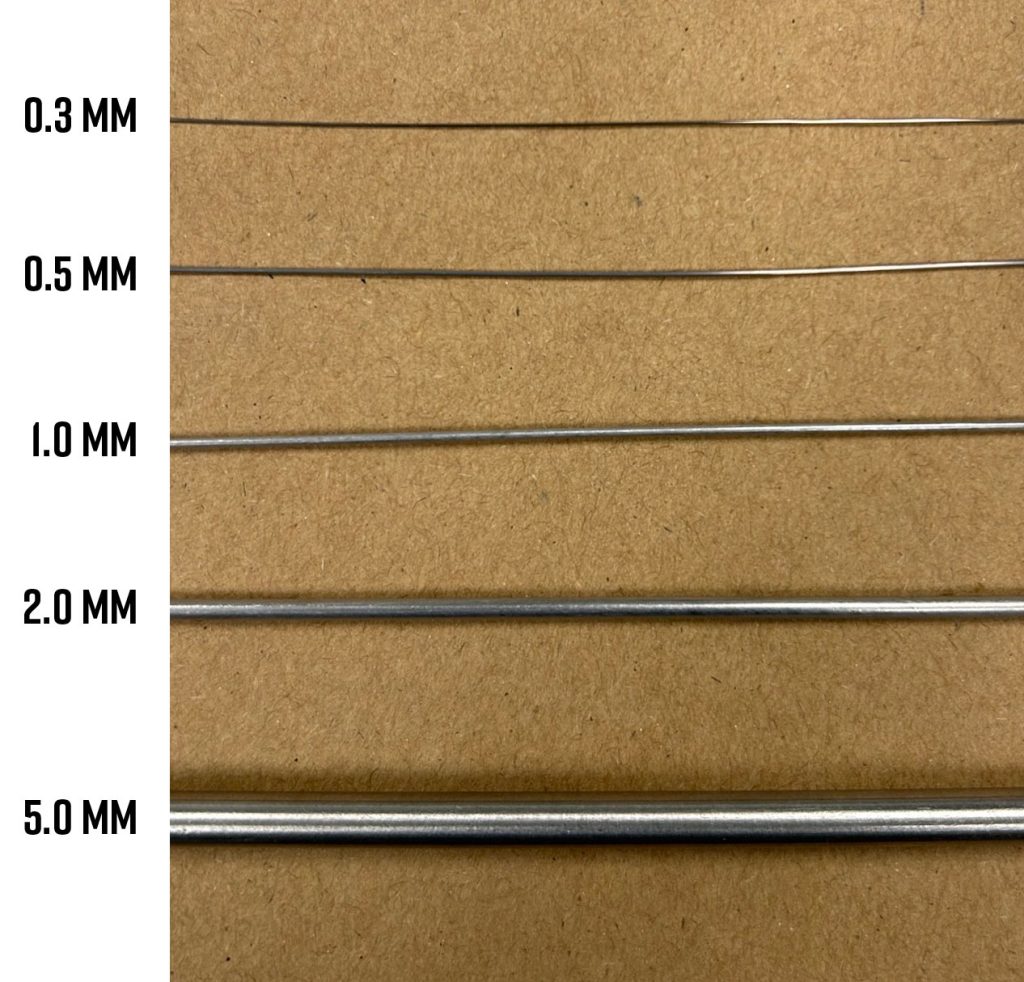
The most common electrospinning setups use a flat plate collector to generate fiber sheets. Alternatively, by electrospinning onto a rotating small-diameter mandrel, electrospun fibers will collect around the circumference of the collector and form a small-diameter tube (Figure 1B). The inner diameter of the tube can be easily controlled by changing the size of the rotating mandrel. This setup can be used to fabricate fibrous tubular structures that can range from 0.3-5 mm in diameter, which is in line with the dimensions necessary for designing small vessel vascular grafts (Figure 2).
Electrospinning for Developing Small-diameter Vascular Grafts
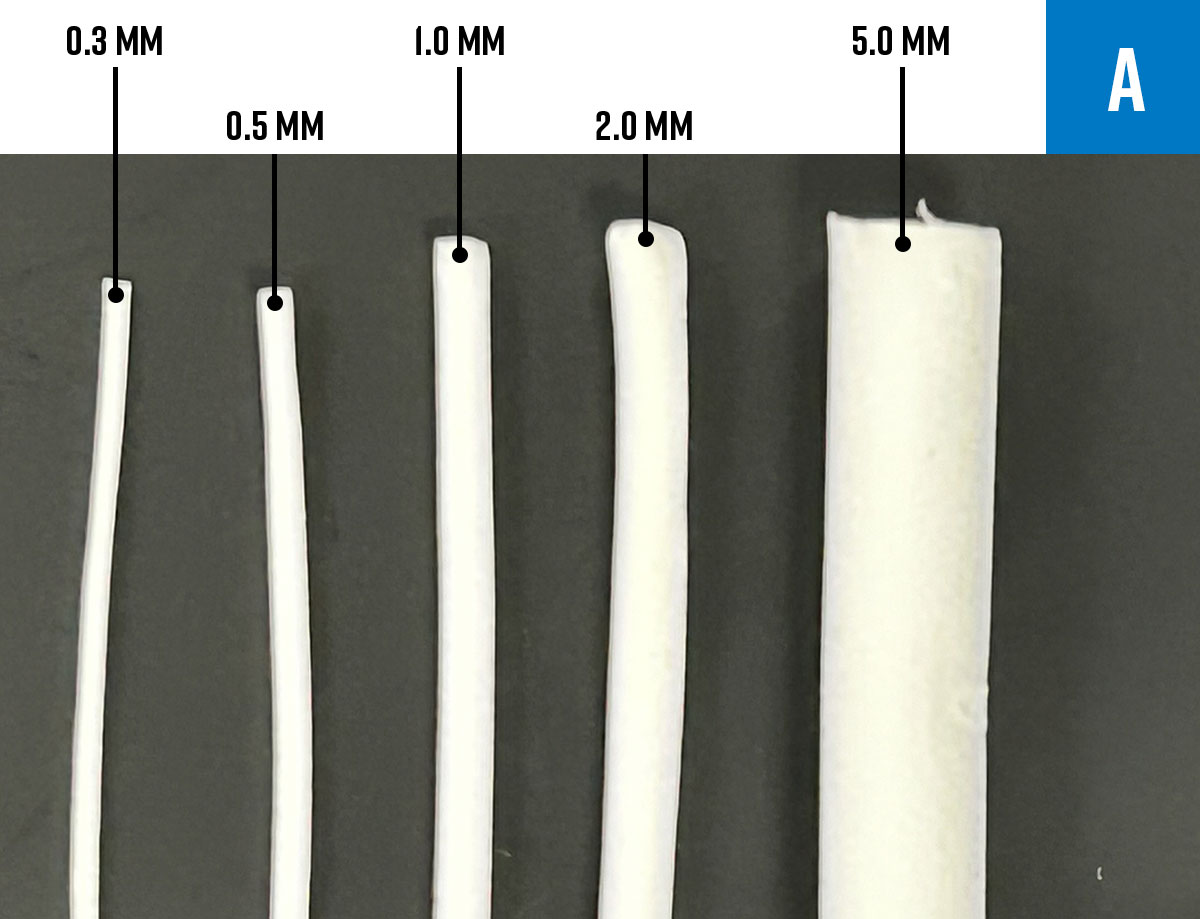
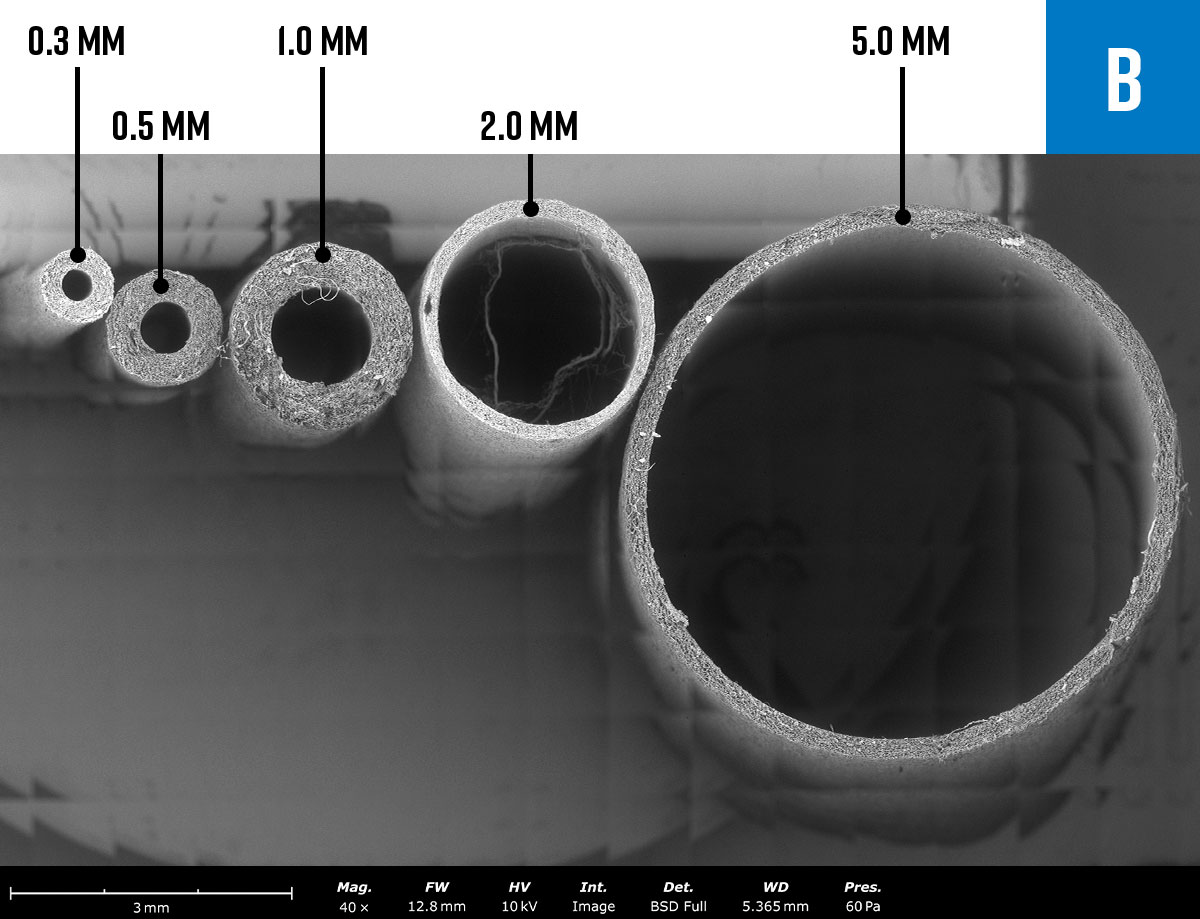
A Fluidnatek LE-100 Biotubing electrospinning system was used with varying sizes of small diameter mandrels to fabricate tubular structures with diameters ranging between 300 µm to 5 mm in inner diameter. Optical images of a segment of the small vascular grafts are seen in Figure 3A. SEM imaging of the cross-sections of each tubular structure confirmed the inner diameter of the tubes fabricated on the different mandrels (Figure 3B). Furthermore, by controlling the electrospinning time, the scaffold wall thickness can be tuned to mimic the diverse wall thicknesses of unique vascular structures (Figure 4).
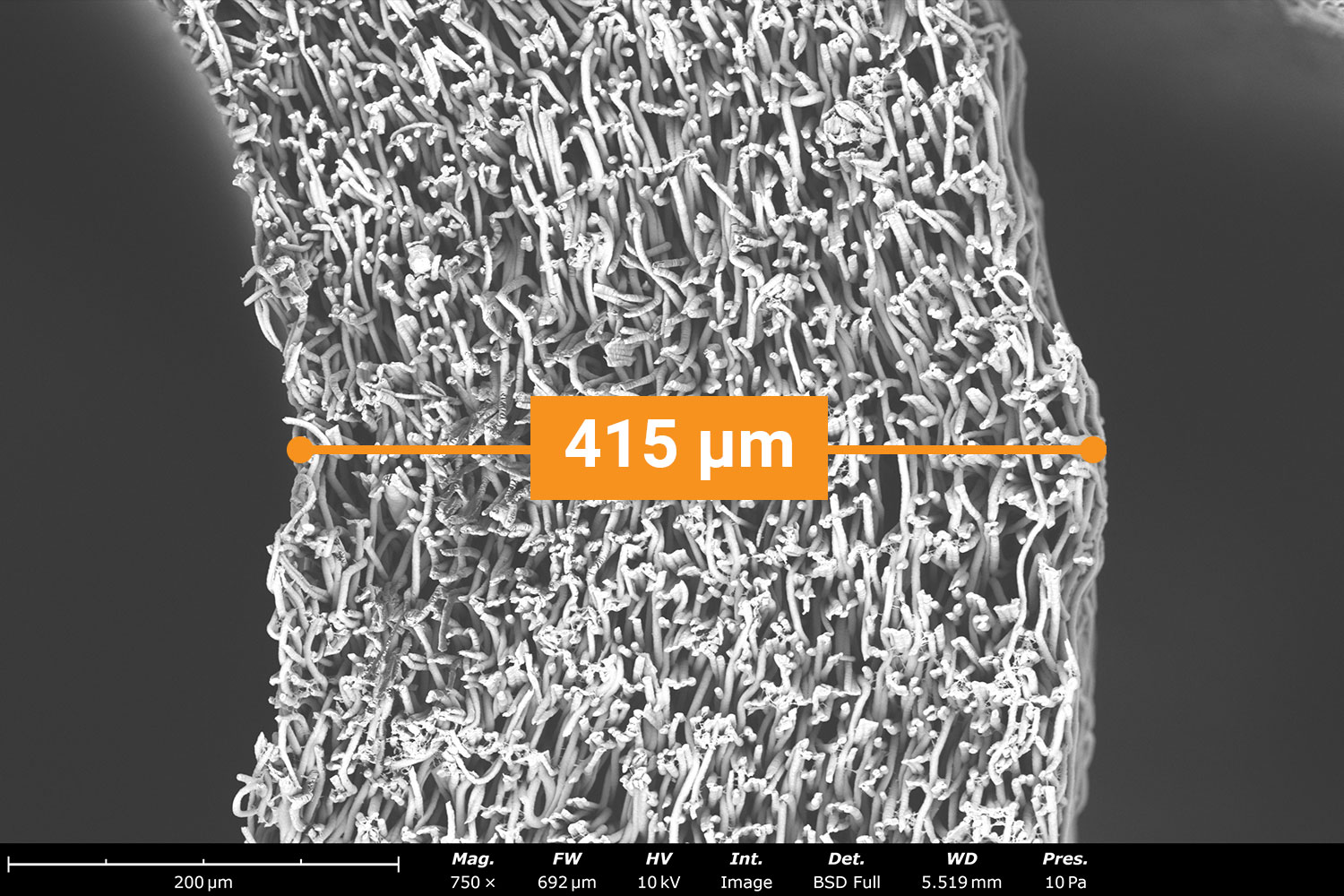
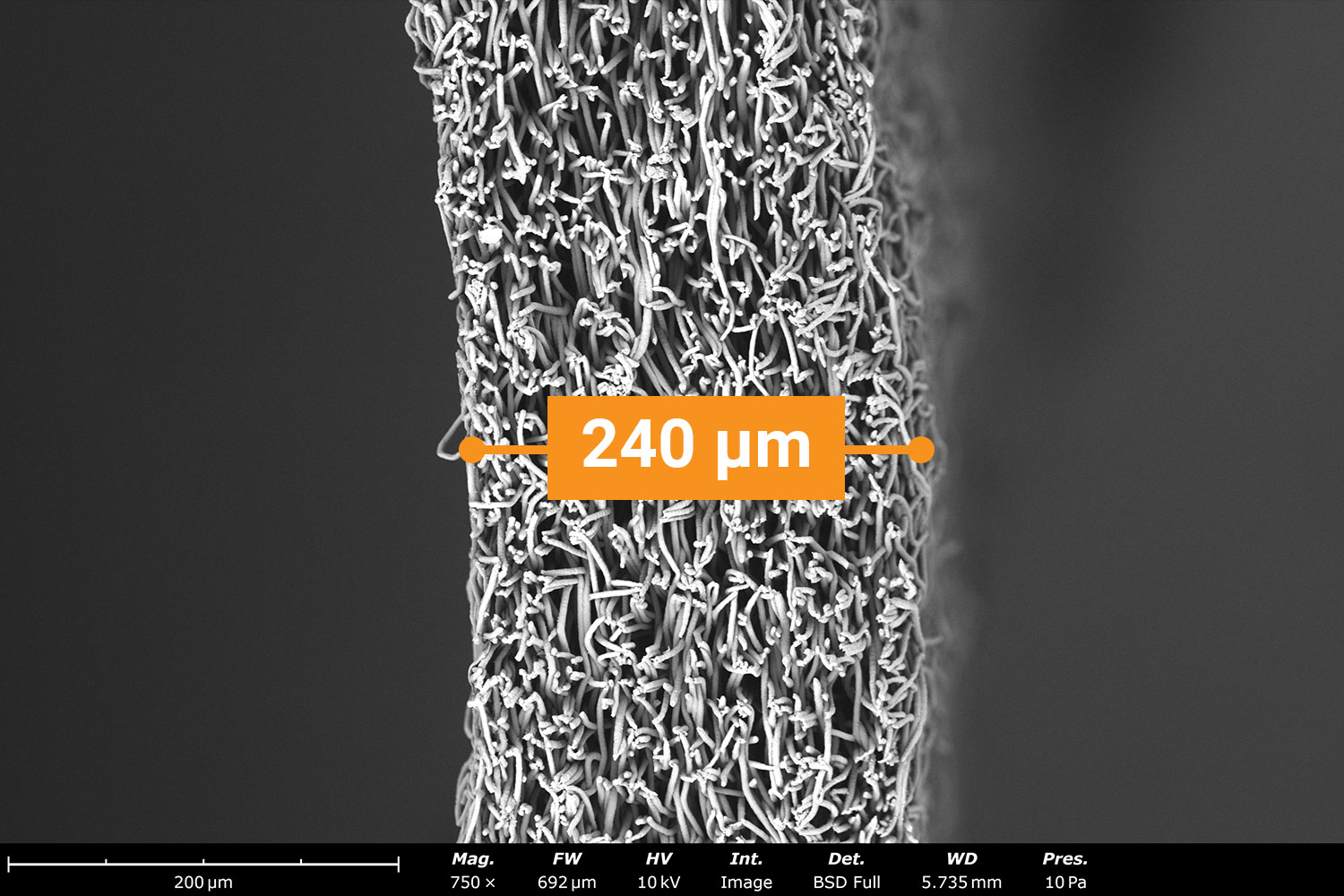
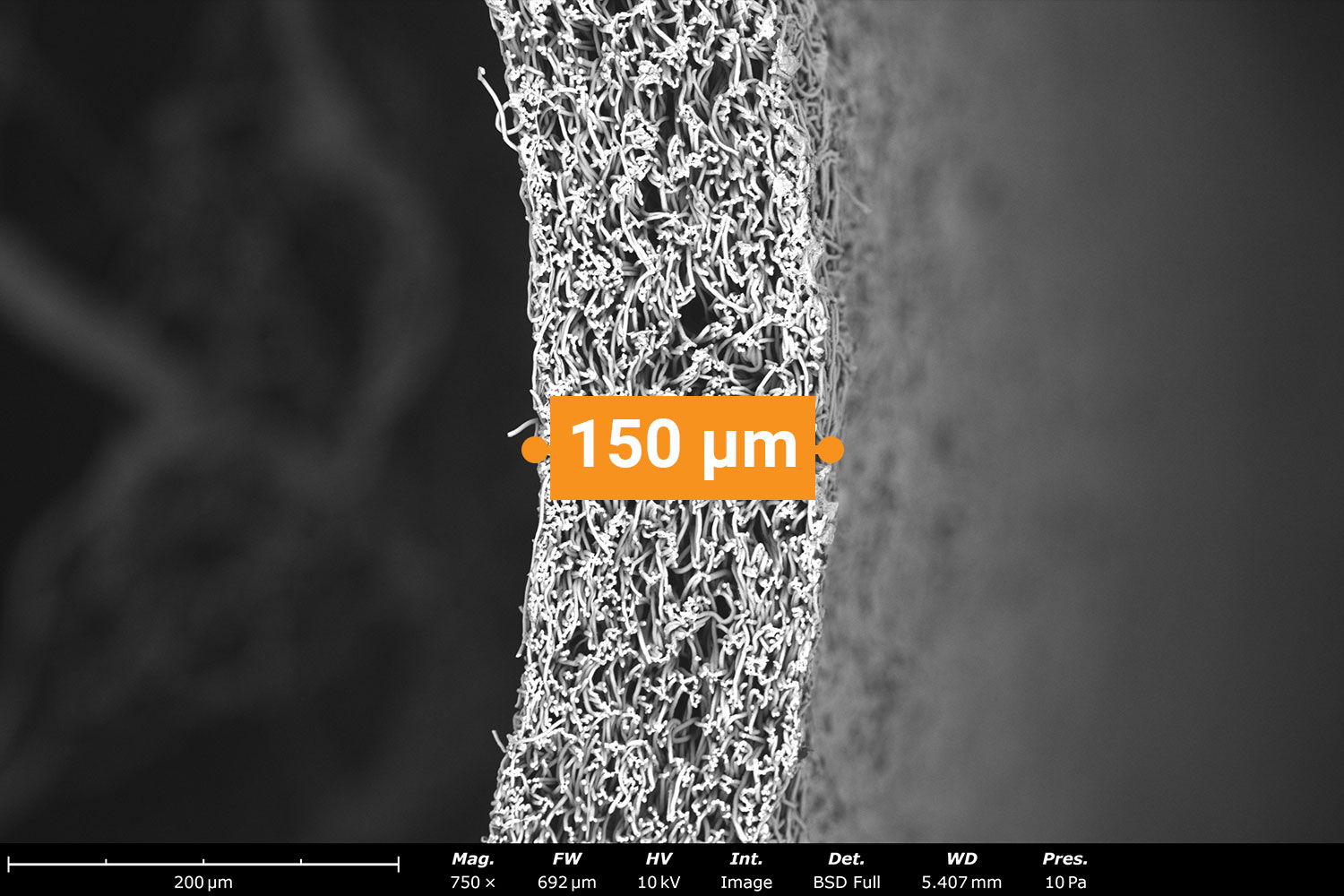
The time required to develop vascular grafts with tunable wall thicknesses depends on the size of the mandrel. For example, a 0.3 mm diameter mandrel has a smaller surface area and requires approximately 5 min to achieve a wall thickness of approximately 200 µm. Achieving the same wall thickness using a 5 mm diameter mandrel will require approximately 30 min. In conjunction with tuning the inner diameter and wall thickness, the vascular grafts can also be designed for various lengths. The LE-100 Biotubing can generate a maximum scaffold length of 35 cm. The wall thickness of the tubular structures will need to be optimized for generating an Electrospun vascular graft with a maximum 35 cm length. Smaller inner diameter grafts may require a higher wall thickness to have enough structural integrity to remove the scaffold from the mandrel.
Conclusion
To prevent the necessity of autologous grafts, it is imperative to develop synthetic vascular grafts that are less than 6 mm in diameter and resistant to thrombosis. Electrospinning onto a small diameter mandrel collector, nanofibrous tubular structures with inner diameters that ranged from 0.3 mm to 5 mm were fabricated. With the capability to Electrospin with antithrombogenic materials; and tune both the inner diameter and wall thickness, these tubular structures can serve as a proper synthetic graft that restores blood flow to small-diameter blood vessels.
References
- Ratner, B. (2023) Vascular Grafts: Technology Success/Technology Failure. BME Front. 2023; 4: 0003. ↩︎
- Atari, M., Saroukhani, A., Manshaei, M., Bateni, P., Vatankhah, E., & Javanmard, S. H. (2023). Preclinical in vivo assessment of a cell-free multi-layered scaffold prepared by 3D printing and electrospinning for small-diameter blood vessel tissue engineering in a canine model. Biomaterials Science, 11(20), 6871-6880. ↩︎
- Li, S., Sengupta, D., & Chien, S. (2014). Vascular tissue engineering: from in vitro to in situ. Wiley Interdisciplinary Reviews: Systems Biology and Medicine, 6(1), 61-76. ↩︎
- Ju, Y. M., Ahn, H., Arenas-Herrera, J., Kim, C., Abolbashari, M., Atala, A., … & Lee, S. J. (2017). Electrospun vascular scaffold for cellularized small diameter blood vessels: A preclinical large animal study. Acta biomaterialia, 59, 58-67. ↩︎
- Wang, Y., He, C., Feng, Y., Yang, Y., Wei, Z., Zhao, W., & Zhao, C. (2020). A chitosan modified asymmetric small-diameter vascular graft with anti-thrombotic and anti-bacterial functions for vascular tissue engineering. Journal of Materials Chemistry B, 8(3), 568-577. ↩︎
- Tindell, R. K., Busselle, L. P., & Holloway, J. L. (2023). Magnetic fields enable precise spatial control over electrospun fiber alignment for fabricating complex gradient materials. Journal of Biomedical Materials Research Part A, 111(6), 778-789. ↩︎
- Yalcin, I., Horakova, J., Mikes, P., Sadikoglu, T. G., Domin, R., & Lukas, D. (2016). Design of polycaprolactone vascular grafts. Journal of Industrial Textiles, 45(5), 813-833. ↩︎
- Song, W., Zeng, Q., Yin, X., Zhu, L., Gong, T., & Pan, C. (2018). Preparation and anticoagulant properties of heparin-like electrospun membranes from carboxymethyl chitosan and bacterial cellulose sulfate. International journal of biological macromolecules, 120, 1396-1405. ↩︎